Ankle Sprains: Don’t Let a Simple Injury Turn into a Long-Term Problem
Ankle sprains are among the most common injuries we see at Praxis Physiotherapy. Whether you’re an AFL midfielder, a cricket fast bowler, or a weekend runner pounding the Brisbane River loop, lateral ankle sprains can derail performance and linger longer than they should.
At Praxis, we’ve rehabilitated hundreds of athletes across all levels, from juniors to pros. Our experience includes long-term roles with the Aspley Hornets AFL Club (since 2014), the Queensland Bulls, Australia A, and even the Australian Men’s Cricket Team. We bring these elite rehab principles to everyone — from sprained-ankle soccer kids to high-performance track athletes.
But despite how common they are, ankle sprains are often underestimated. Without proper rehab, they can lead to chronic ankle instability (CAI), impaired athletic performance, and even new injuries in other parts of the body.
What Actually Happens in an Ankle Sprain?
A lateral ankle sprain usually occurs when the foot rolls inward, stretching or tearing the ligaments on the outside of the ankle — most commonly the anterior talofibular ligament (ATFL). It often happens during sudden changes of direction, awkward landings, or stepping on uneven ground.
You might feel a pop or crunch, followed by swelling, bruising, and pain when walking or bearing weight. While it may seem like a “simple sprain,” it’s anything but — around 40% of people report long-term issues one year post-injury if not managed well.
Common Mistake: Rest, Ice, and… That’s It?
Too many people still follow the old R.I.C.E. (rest, ice, compression, elevation) model and assume the job is done. While these strategies can help in the first 48 hours, they’re far from sufficient for full recovery.
In fact, research has shown that inadequate rehab is a major contributor to chronic ankle instability — a condition marked by recurrent sprains, feelings of the ankle “giving way,” and reduced confidence in movement.
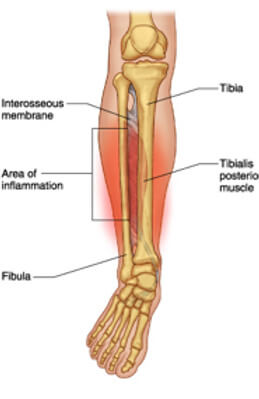
CAI can lead to altered biomechanics and poor neuromuscular control, increasing the risk of knee injuries, Achilles tendinopathy, or even hip and low back pain due to compensation.
Proper Rehabilitation Is Key — Here’s What the Evidence Says
Rehabilitation needs to start early and be progressive. High-quality clinical guidelines and systematic reviews strongly support the following strategies:
Functional Support and Early Mobilisation
Functional bracing (like an ankle brace or taping) is preferred over rigid immobilisation and should be used for 4–6 weeks . Early weight-bearing as tolerated leads to quicker return to activity and better outcomes .
Exercise Therapy
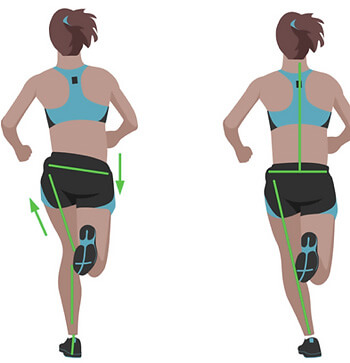
Neuromuscular training (balance, proprioception, and strength work) is the foundation of successful rehab. It improves ankle control, prevents recurrence, and reduces the risk of CAI. A wobble board, single-leg balance, hopping drills, and directional change exercises are all commonly used.
Manual Therapy
Joint mobilisations and soft tissue work may improve dorsiflexion range, decrease pain, and aid in functional recovery. At Praxis, we combine manual therapy with functional retraining to fast-track performance readiness.
Individualised Return-to-Sport Testing
Return to sport shouldn’t be based on time alone. We use objective testing — including single-leg hop symmetry, balance tests, and strength assessments — to ensure you’re not returning with deficits that could increase your reinjury risk.
The Cost of Incomplete Rehab: What Happens If You Don’t Get It Right?
A rushed or poorly structured rehab may get you back to activity temporarily — but it opens the door to:
Chronic Ankle Instability (CAI): Repeated sprains, perceived instability, and loss of ankle confidence.
Performance Limitations: Reduced agility, speed, and power due to poor proprioception and strength deficits.
New Injuries: Compensatory patterns can lead to medial tibial stress syndrome (shin splints), Achilles overload, or even ACL risk due to poor landing mechanics.
In elite sport, we see this cascade far too often. That’s why our rehab at Praxis isn’t just about the ankle — it’s about restoring whole-limb function and confidence under pressure.
Prevention: Keep Your Ankles Bulletproof
At Praxis Physiotherapy, we don’t just treat ankle sprains — we help prevent them. Our prevention approach includes:
Regular Balance and Plyometric Training: Incorporating single-leg exercises into gym and field work.
Proprioceptive Work: Using wobble boards, balance mats, and directional hopping.
Footwear and Bracing Advice: Particularly for high-risk sports like netball, football, and athletics.
Pre-season Screening and Performance Testing: For our affiliated sports clubs and athletic populations.
Evidence supports proprioceptive training as a proven strategy to reduce ankle sprain incidence by up to 35% in high-risk athletes.
Why Choose Praxis Physiotherapy?
Our exposure to elite sport has taught us what good rehab looks like — and we apply those same high standards to every patient. Our clinics are equipped with strength testing tools, reformer Pilates, and full gym access, giving you the tools to rebuild better.
We understand the mindset of athletes — from juniors chasing state squads to elite-level players returning from surgery. That’s why we tailor your program based on sport demands, movement patterns, and individual goals.
Whether you rolled your ankle playing touch footy or twisted it at work, we’re here to get you back — stronger, faster, and more confident than before.
Need Help with an Ankle Sprain?
If you’ve recently rolled your ankle or are dealing with ongoing instability, book a consultation at Praxis Physiotherapy. Let our team guide you through a structured rehab program grounded in sports science and elite clinical standards.
📍 Clinics in Teneriffe, Buranda, and Carseldine
💪 Trusted by athletes. Backed by evidence. Here for every body.
References
Ruiz-Sánchez et al. (2022). Management and treatment of ankle sprain according to clinical practice guidelines: A PRISMA systematic review. Medicine (Baltimore), 101(42)
Green et al. (2019). What is the quality of clinical practice guidelines for the treatment of acute lateral ankle ligament sprains in adults? BMC Musculoskeletal Disorders, 20(394)
Doherty et al. (2017). Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. BJSM, 51(2), 113–125.