Peri-Menopause and injury – your guide to the most common issues
- Menopause alters hormones and results in physical changes
- These changes typically result in increased injury risk or activity reduction
- The most common injuries affect structures such as the plantar fascia, tendons of the hip and shoulder
- Appropriate exercise and judicious hands on therapy should be cornerstones of management
Heel pain – Plantar fasciopathy (the injury formerly known as plantar fasciitis)
Heel pain can be a number of things. The heel pain that I tend to see the most of is the one that feels like you are walking on glass the first thing in the morning or after you have been sitting down for a while. It makes you walk like your Grandma used to for those first few steps and the thought of doing a long walk, or heaven forbid wearing heels, gives you the sweats.
This pain is usually characterized by a condition called plantar fasciopathy. The plantar fascia is designed to help to absorb, store and transfer force during walking, running and jumping activities. Collagen (the main protein based building blocks of the body) is a non contractile tissue that sits on the underside of your foot. The attachment point for this tissue, is you guessed it, on the bottom of your heel where that “burning glass” feeling .
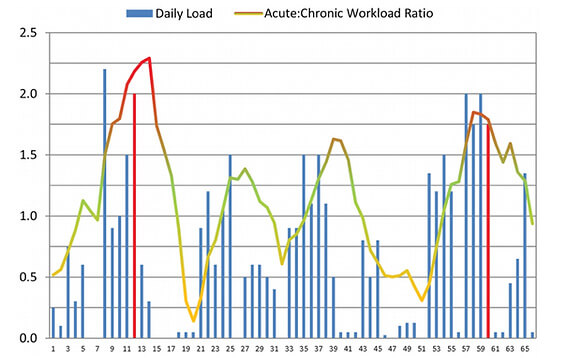
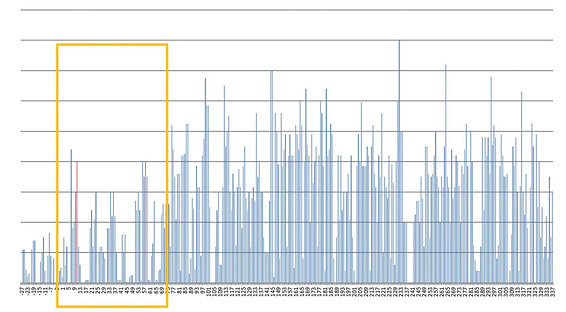
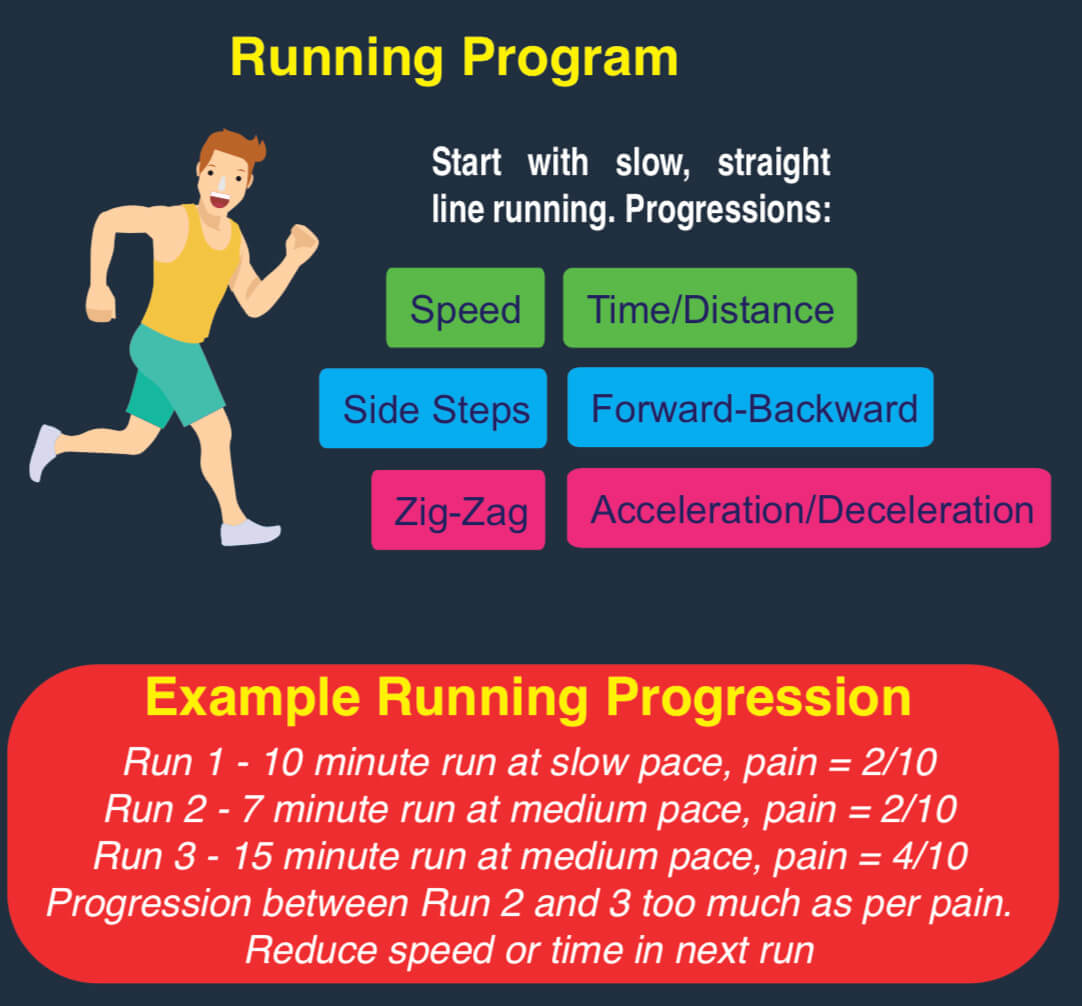
Plantar fasciopathy loves the status quo. It likes loading the same way, at the same intensity, at the same volume day in day out. Pain and dysfunction is brought about typically in a sudden increase in dynamic loading, whether that is walking, running or jumping. This often happens with women hell bent on a health kick to lose those extra kilos. With the shoelaces tied, lycra on and the world your oyster, some women start at where they remember they left their exercise behind, often several years (and children) ago. The resultant spike in load, particularly dynamic loading coupled with musculoskeletal detraining, is what kicks off the pain as the plantar fascia gets overloaded more easily and grizzles about it.
Key tip – Start slow with walks – not running – if it has been a while since you last exercised. Progress to jogging with some walk intervals in there (e.g 30s jog, 90s walk). Do calf raises (eg. 3 sets to a feeling of semi-fatigue) to get more calf strength as this can help deload the plantar fascia.
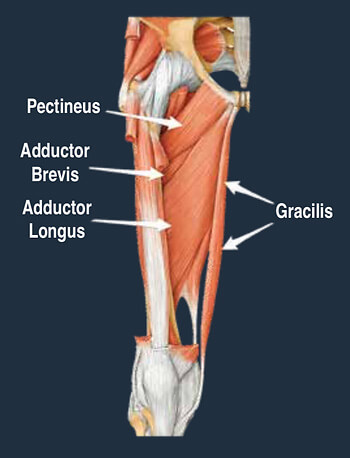
Outside / Lateral hip pain (Gluteus medius tendinopathy)
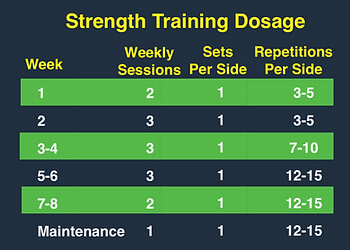
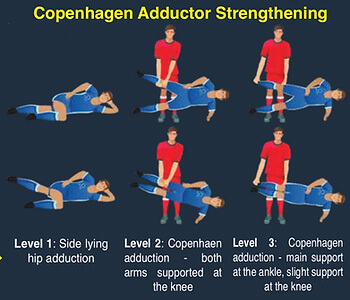
The muscles on the outside of your hips are designed to help keep your pelvis level when you are walking or running. This area is a particular passion of mine given my masters thesis was based on the single leg squat. Similar to the plantar fasciopathy, gluteal tendinopathies tend to be an injury that I see when people go too hard, too quickly. This results in outside hip pain that hurts rising from a chair, walking up stairs or even lying on that side at night.
The human instinct is to rest, but tendinopathies don’t work that way, in fact it is the opposite. The only way to adequately address issues such as gluteal tendinopathy is getting on top of your workload. Ensure you are graduating whatever activity you are re-engaging in appropriately, and you have the strength to do so. I typically use a hand held dynamometer in my clinic to assess someone’s strength to give me accurate numbers to work with. However, a rough guide is that if you can do a side plank for 30 seconds, you need some more hip strength.
Key tip – Workload management and pain management are paramount. If in pain, reduce loading and focus on strength. Lying hip lifts (e.g. 10 x 10 sec holds) are good when pain is acute. If not sore (just weak), side plank with top leg lifts are a good option to start. 3 x semi-fatigue each side. We employ reformer pilates often in this space but gym based activities are also appropriate.

Shoulder Pain – “Rotator Cuff” tears / tendinopathy
Do you have a ‘good’ and ‘bad’ shoulder? Have you been putting up with that grumbly shoulder for weeks, months or even years? Shoulder pain can put a real dampener on activities where repetitive overhead dynamic loading is common (e.g weights, tennis, golf or boxing).

The “rotator cuff” is a group of four muscles that help provide stability and control of the shoulder joint through range, particularly overhead. Rotator cuff tears are common in individuals over the age of 40 with linear increase in incidence as we get older. The most common reason for rotator cuff tears are due to overactivity of the shoulder joint coupled with deconditioning of the shoulder complex. Pain with movement and function is one of the biggest symptoms of a rotator cuff pathology.
Key Tip – Look at how much overhead activity you are doing and adequately prepare for it. This is best achieved in my experience with something like a banded Y Press hold (10x10s holds daily for a month) then progressing to more dynamic activities.
All in all, changes associated with menopause can leave you open to more injuries. However, if you can appropriately navigate, and most importantly graduate, your return to physical activity, then your body will certainly pay you dividends down the line. The evidence is overwhelming for the positive influences physical has on the human body. So do yourself (and your future self) a favour and ensure you aren’t retreating from your physical activity goals due to injury. It’s not what Betty would want.
If you have some of the above aches and pains, feel free to reach out or book in with one of our expert therapists.
Until next time, Praxis what you Preach.
Stephen Timms
All information is general in nature and it is always best to see your local physiotherapist, who uses exercise as the cornerstone of your rehabilitation.