SUMMARY:
- Stingers are essentially a tractioning of the neural system
- This can cause pain, movement and sensation changes
- Chronic traction to the nervous system can have a cumulative effect on nerve function
- The more damage to the nerve, the more serious the outcome
- We shouldn’t be as dismissive of “stingers”, particularly if they are recurrent
- Physiotherapy has a role to play
STINGERS:
Stingers have been the catch cry of many contact sports over the years. Often dismissed as ‘just a stinger’, trauma to the nervous system should probably be taken a little more seriously, as we delve into detail today.
Stingers are most commonly experienced in contact sports whereby the shoulder of a players is forcefully depressed, as experienced with a tackle in NRL or union. A large range of motion over a short period of time can result in a ‘traction’ of the Brachial Plexus (a network of nerves formed from exiting branches of the spinal cord in the neck that transverse to the shoulder and arm). Thus network of nerves sends signals from your spinal cord to your shoulder, arm and hand and thereby providing feeling and movement to these regions.
BACKGROUND:
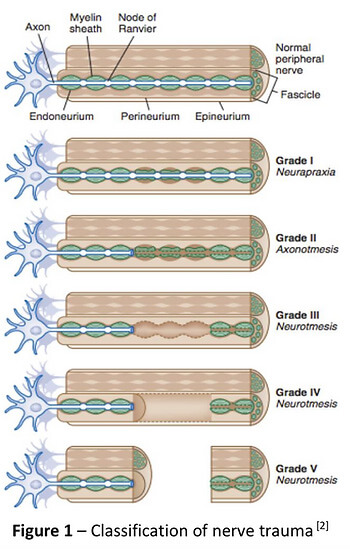
To understand a stinger injury, a clear understanding of nerves and nerve related injuries is required. A nerve is an enclosed, cable-like bundle of nerve fibres called axons, in the peripheral nervous system. A nerve provides a common pathway for the electrochemical nerve impulses that provide a number of functions, including getting our muscles to move!
Seddon and Sunderland present a five-grade classification scale for nerve related injuries[1-4]. Figure 1 illustrates the physiological changes that occur through each grade of injury. Essentially it outlines the greater amount of disruption to the anatomy of the nerve.
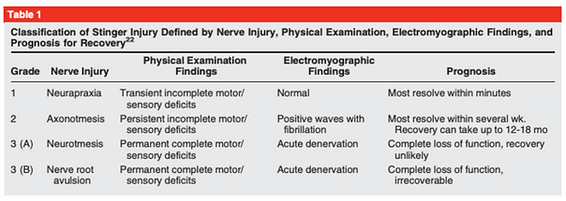
The more damage to the nerve, the more serious the outcome. Table 1 outlines the three different grades of stinger injuries.[4, 5] The most common stinger is a grade 1 injury, which represents a neurapraxia, or nerve stretch injury, without axonal disruption.[4] In an acute setting, this can result in motor and sensory loss/changes, which usually resolve within minutes.[1, 4] Grade 2 and 3 involve a higher degree of nerve injury, usually involving a crush, transection or compression mechanism.[1]
Chronic traction to the nervous system can have a cumulative effect on nerve function. This is termed “chronic stinger syndrome” and represents a distinct entity from acute stingers that may reflect long- standing structural changes of the subaxial spinal canal and chronic irritation/degeneration of the exiting nerve root complex.[4, 6]. This sounds complex but essentially means
A Clinical Example from Zac
“During a Gridiron match, a player was injured whilst making a tackle. I reviewed the player on field and he was unable to utilise his right upper limb (full paralysis) from shoulder down to his hand. The player was removed from the field immediately to be further assessed and monitored. A complete neurovascular assessment was performed, assessing motor function/strength, sensation, reflexes, and vascular status, as well was the cervical spine. Motor and sensation changes were the only deficits noted and were reviewed frequently. After roughly five minutes, the player demonstrated full upper limb motor strength and sensation, with nil lingering symptoms. In collaboration with the patient, it was decided he would return to match play immediately. The patient was monitored throughout the game and reported no further symptoms.”
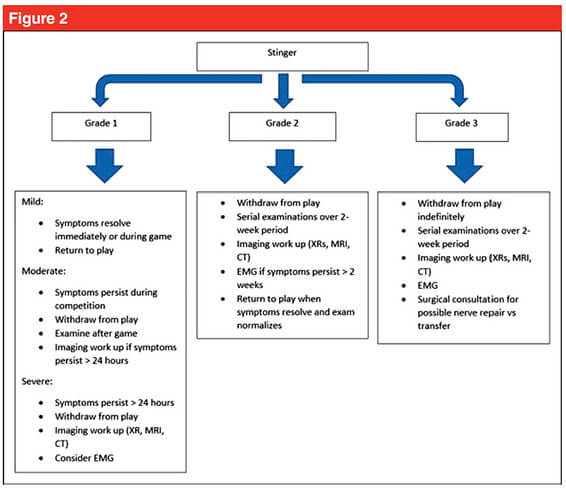
Figure 2 shows a proposed decision tree when managing stinger injuries.[4] This clinical example outline above fits the Grade 1 Mild category as he was able to return to competition with nil lingering symptoms. Despite the lack of symptoms during the game, it is recommended the patient be reviewed again both after the game and weekly for two weeks to ensure a full resolution of symptoms.[4, 7]
The role for neural mobilisation?
Current non-surgical management involves rest, pain control and resistance training[4]. Though not explored within the literature, neural mobilization may have an important role in patients with persistent symptoms, such as Grade 1 moderate to severe, and more recurrent neuropraxias. Though not assessed in this specific population, there is evidence for neural tissue management being superior to minimal intervention for pain relief and reduction of disability in nerve related chronic musculoskeletal pain.[8] It is biologically plausible that recurrent neuropraxias may respond in a similar way, utilising neural mobilisation (tensioning or sliding) and mobilisation of surrounding structures.
Management of persistent Grade 1 injuries may differ slightly, specifically if the suspected mechanism of injury was through traction rather than compression. The nerve structures may have a heightened sensitivity to tensioning based techniques due to the similar mechanism of injury and may respond better acutely to sliding techniques which limit the strain on the nerve and focus on excursion. Tensioning techniques may be important in the sub-acute phase by loading the patient’s nervous system (i.e. increased strain) in preparation for return to function (i.e. tackling with acute traction on the brachial plexus).
In summary, perhaps we shouldn’t be as dismissive of “stingers”, particularly if they are recurrent for you! If you have any questions or would like to see one of our physios regarding your injury, feel free to contact us on (07) 3102 3337 or book online on our website
Till next time, Praxis what you Preach
Team Praxis
Prevent | Prepare | Perform
REFERENCES:
Menorca, R.M.G., T.S. Fussell, and J.C. Elfar, Nerve physiology: mechanisms of injury and recovery. Hand clinics, 2013. 29(3): p. 317-330.
Tsao B, B.N., Bethoux F, Murray B, Trauma of the Nervous System, Peripheral Nerve Trauma. 6th ed. In: Daroff: Bradley’s Neurology in Clinical Practice. 2012.
Sunderland, S., A classification of peripheral nerve injuries producing loss of function. Brain, 1951. 74(4): p. 491-516.
Ahearn, B.M., H.M. Starr, and J.G. Seiler, Traumatic Brachial Plexopathy in Athletes: Current Concepts for Diagnosis and Management of Stingers. J Am Acad Orthop Surg, 2019.
Feinberg, J.H., Burners and stingers. Phys Med Rehabil Clin N Am, 2000. 11(4): p. 771-84.
Presciutti, S.M., et al., Mean subaxial space available for the cord index as a novel method of measuring cervical spine geometry to predict the chronic stinger syndrome in American football players. J Neurosurg Spine, 2009. 11(3): p. 264-71.
Aldridge, J.W., et al., Nerve entrapment in athletes. Clin Sports Med, 2001. 20(1): p. 95-122.
Su, Y. and E.C. Lim, Does Evidence Support the Use of Neural Tissue Management to Reduce Pain and Disability in Nerve-related Chronic Musculoskeletal Pain?: A Systematic Review With Meta-Analysis. Clin J Pain, 2016. 32(11): p. 991-1004.