Shin Splints: Causes, Treatment & How to Get Back to Running Stronger
Key Takeaways
Shin splints (MTSS) are an overuse bone stress injury.
Training load errors are the biggest contributor.
Hip strength and force control play a major role.
Early management prevents stress fractures.
Strength + smart loading beats rest alone.
Shin Splints
Shin splints, known in the research as medial tibial stress syndrome (MTSS) are one of the most common running injuries we see at Praxis Physiotherapy across our Teneriffe, Buranda and Carseldine clinics.
If you’re noticing a dull ache along the inside of your shin that worsens with running, skipping or sport, you’re not alone. The good news? With the right plan, shin splints are highly manageable — and preventable.
Let’s break down what’s actually happening, why it develops, and what you can start doing today.
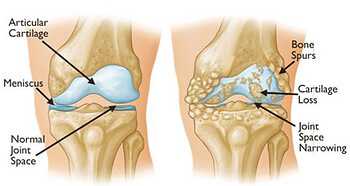
What Are Shin Splints (Medial Tibial Stress Syndrome)?
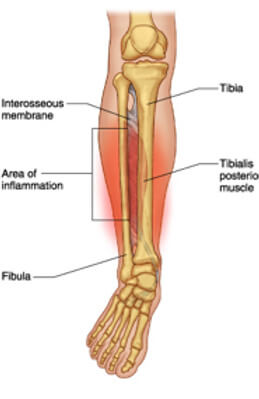
Shin splints are an overuse bone stress injury affecting the inner (medial) border of your tibia (shin bone).
What does it feel like?
Aching pain along the lower inside shin
Sharp pain when running or jumping
Tenderness to touch along the bone
Morning stiffness or pain when first starting activity
Unlike a stress fracture (which is more focal and severe), shin splints usually present as a broader area of tenderness along the bone.
What’s Actually Happening? (The Pathology Explained Simply)
MTSS is no longer thought to be just an “inflammation” problem.
Current evidence suggests shin splints develop due to repetitive loading that exceeds the bone’s capacity to adapt. When running loads increase too quickly, the tibia experiences repeated bending stress. If recovery isn’t adequate, this leads to:
Bone stress reaction
Irritation of the periosteum (bone lining)
Localised pain along the medial tibia
If ignored, MTSS can progress to a tibial stress fracture, which requires significantly longer time away from running.
That’s why early management matters.
Why Do Shin Splints Develop?
A large systematic review by Winkelmann et al. (2016) identified over 100 potential risk factors for MTSS, with several consistently seen in clinical practice.
Key Risk Factors Supported by Research
1. Training Load Errors
Rapid increases in running volume, intensity, or frequency are one of the strongest contributors.
(Winters et al., 2013; Nielsen et al., 2012)
2. Higher Body Mass Index (BMI)
Greater body mass increases tibial loading forces.
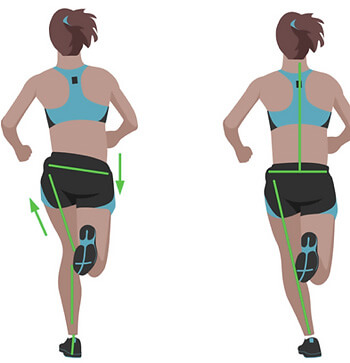
3. Biomechanical Factors
Increased navicular drop (foot pronation)
Greater plantarflexion range
Hip muscle weakness and poor pelvic control
4. Previous History of MTSS
Recurrence risk is higher without proper rehabilitation.
Importantly flat feet alone are rarely the sole cause.
What we often see clinically is this chain reaction:
Poor hip control → knee collapses inward → foot over-pronates → increased traction stress on medial tibia.
The foot is often the victim, not the culprit.
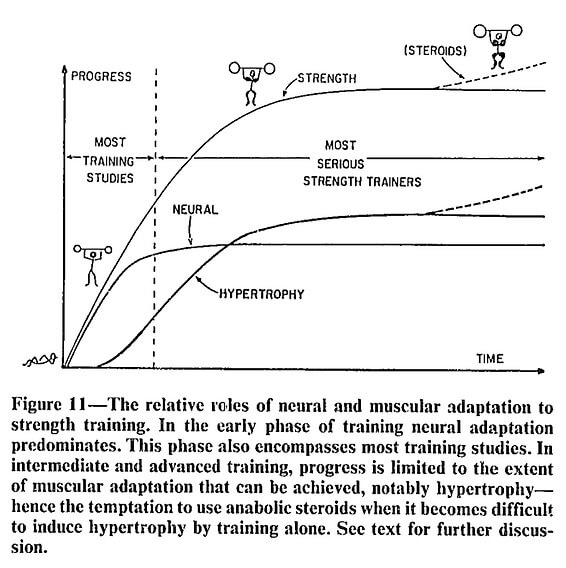
Why Rest Alone Isn’t Enough
Yes — rest reduces pain. But rest does not improve:
Load tolerance
Running capacity
Strength deficits
Movement control
This explains why shin splints are common in recreational runners but less frequent in well-structured training programs. Higher-level athletes typically follow progressive loading plans that allow bone and tendon adaptation.
Research consistently supports graded loading and strengthening as key components of recovery (Moen et al., 2012).
.

How to Manage Shin Splints (Early Stage Tips)
If your symptoms are mild to moderate, here are evidence-informed starting points:
1️⃣ Relative Rest (Not Complete Rest)
Reduce running volume by 30–50%.
Avoid sharp increases in load.
Swap some runs for cycling or swimming temporarily.
2️⃣ Strengthen the “Shock Absorbers”
Focus on:
Calf strength (bent and straight knee)
Tibialis posterior strengthening
Glute medius and hip control exercises
Single-leg stability work
Improving hip strength can reduce tibial loading by improving force control through the limb.
3️⃣ Manage Running Workload
Follow the “10% rule” cautiously.
Allow recovery days between harder sessions.
Avoid sudden terrain changes (e.g., grass → concrete).
4️⃣ Consider Footwear
Ensure shoes are not worn out (>600–800km).
Orthotics may help some individuals — but only after assessment.
When Should You See a Physio?
Seek professional assessment if:
Pain persists longer than 2–3 weeks
Pain becomes sharp and localised
Hopping on one leg is painful
Symptoms worsen despite reducing load
Early intervention reduces the risk of progression to stress fracture.
How Praxis Approaches Shin Splints
At Praxis, we don’t treat “shin splints.”
We treat your specific loading problem.
Your plan may include:
✔ Comprehensive running and strength assessment
✔ Individualised load management plan
✔ Targeted strength and control program
✔ Manual therapy where appropriate
✔ Gradual return-to-run progression
✔ Prevention strategy for long-term performance
Because no two runners load the same way, and no two recovery plans should be identical.
If you’re dealing with shin splints, or want to prevent them from coming back, our team can help.
Book an in-depth running and lower limb assessment today.
📍 Clinics in Teneriffe, Buranda & Carseldine
📞 (07) 3102 3337
💻 Book online
💪 Trusted by athletes. Backed by evidence. Here for everyone.
The Praxis Team.
PREVENT | PREPARE | PERFORM
References
Winkelmann ZK et al. (2016). Risk factors for medial tibial stress syndrome in active individuals. Journal of Athletic Training, 51(12), 1049–1052.
Winters M et al. (2013). Medial tibial stress syndrome: a critical review. Sports Medicine, 43(12), 1315–1333.
Moen MH et al. (2012). Treatment of medial tibial stress syndrome: a systematic review. Sports Medicine, 42(11), 965–981.
Nielsen RO et al. (2012). Training errors and running-related injuries. International Journal of Sports Physical Therapy, 7(1), 58–75.
Images:
The above images are owned by the “Trainer Academy (https://traineracademy.org/) ” and used in this article with thanks.
References:
- Hopper D, Deacon S, Das S, et al. Dynamic soft tissue mobilization increases hamstring flexibility in healthy male subjects. Br J Sports Med. 2004;39:594–598
- Weerapong, P., Hume, P.A. & Kolt, G.S. The mechanisms of massage and effects on performance, muscle recovery and injury prevention. Sports Med 2005; 35: 235
- Morelli M, Seaborne DE, Sullivan SJ. Changes in h-reflex amplitude during massage of triceps surae in healthy subjects.J Orthop Sports Phys Ther. 1990;12(2):55-9.
- Arroyo-Morales M1, Fernández-Lao C, Ariza-García A, Toro-Velasco C, Winters M, Díaz-Rodríguez L, Cantarero-Villanueva I, Huijbregts P, Fernández-De-las-Peñas C. Psychophysiological effects of preperformance massage before isokinetic exercise. J Strength Cond Res. 2011 Feb;25(2):481-8.
https://www.massagemyotherapy.com.au/Home