
Why Tennis Elbow Takes So Long to Get Better (And What Actually Works)

Ifyou’ve had tennis elbow (also called lateral epicondylalgia), you’ll know it’s not just a “sore elbow.”It’s pain when lifting a coffee cup. Pain shaking hands. Pain turning a door handle. Pain gripping the gym bar or picking up your kids.
And frustratingly, it can hang around for months. So why does tennis elbow take so long to improve? And are injections like cortisone really the quick fix people hope they are?
Let’s unpack it during this installment of Praxis What You Preach
First — It’s Not Really “Inflammation”
Despite the name lateral epicondylitis, most modern research shows that tennis elbow is not primarily an inflammatory condition.
Histological studies consistently demonstrate degenerative tendon changes such as disorganised collagen, increased fibroblasts and vascular changes — rather than classic inflammatory cells. In other words, it’s more accurate to call it a tendinosis or tendinopathy rather than a true “-itis” condition (Herd & Meserve, 2008; Pathan & Sharath, 2023).
This distinction matters. Inflammatory problems (like a sprained ankle in the first few days) often respond quickly to anti-inflammatory treatments.
Degenerative tendon problems do not.
What’s Actually Happening?

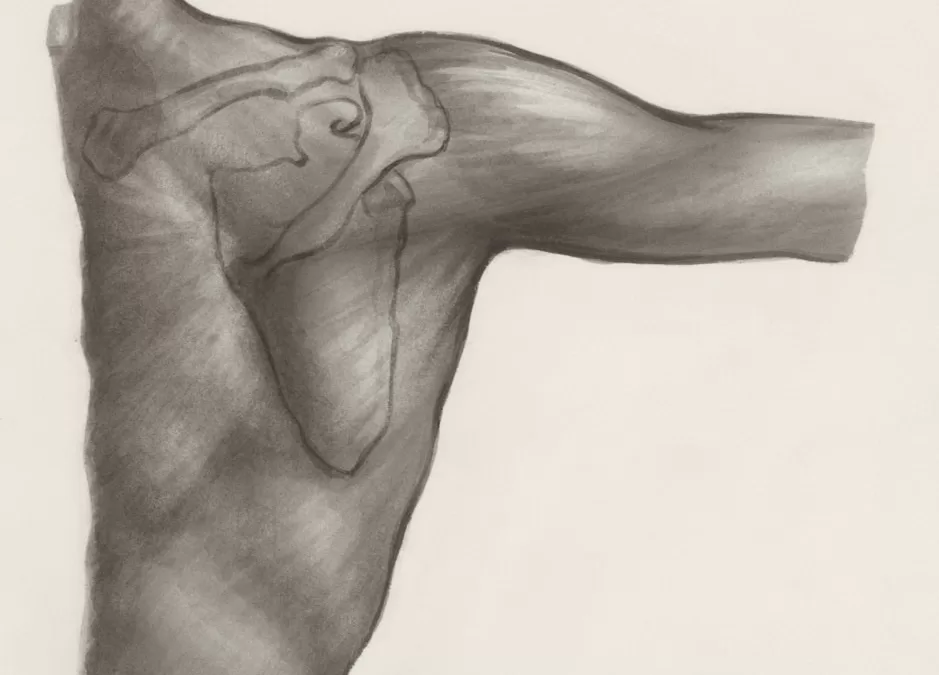
In around 90% of cases, the extensor carpi radialis brevis (ECRB) tendon is involved (Pathan & Sharath, 2023). This tendon is heavily loaded during gripping and wrist extension — especially repetitive tasks like typing, manual labour, racquet sports, or gym training.
Over time, repeated micro-loading can exceed the tendon’s capacity. When the tendon fails to adapt effectively, it begins to:
- Lose collagen organisation
- Develop microtears
- Show reduced tensile capacity
- Become painful with load
This process develops gradually. And that’s one key reason recovery isn’t instant.
“But I’ve Rested It — Why Is It Still Sore?”
Because tendons don’t heal well with complete rest. They need progressive, appropriate load to stimulate remodelling.
Without mechanical stimulus:
- Collagen alignment worsens
- Tendon capacity reduces
- Grip strength declines
- Pain can actually persist longer
This is why high-quality physiotherapy programs focus on graded strengthening, tendon capacity rebuilding, and load modification, rather than pure rest (Pathan & Sharath, 2023; Yelland et al., 2019).
Natural History: Does It Just Go Away?
Tennis elbow is often described as “self-limiting.” Some reports suggest many cases improve within 8–12 months (Houck et al., 2019), and older literature even suggested high rates of improvement at one year (Herd & Meserve, 2008).
However, that doesn’t mean:
- It resolves quickly
- It resolves optimally
- It resolves without recurrence
- It resolves without strength deficits
Up to 10% of patients develop persistent symptoms severe enough to consider surgery (Yelland et al., 2019).
And in working adults, particularly manual workers, the functional and economic impact is significant.
So while time helps, structured intervention helps more.
What About Cortisone Injections?
 Corticosteroid injections are still widely used for tennis elbow. They are:
Corticosteroid injections are still widely used for tennis elbow. They are:
- Relatively inexpensive
- Quick to administer
- Often very effective for short-term pain relief
And the evidence supports that. Multiple systematic reviews demonstrate that corticosteroid injections are more effective than other treatments in the short term (typically under 12 weeks) (Houck et al., 2019).
The problem? The long term. The same high-level evidence shows that corticosteroid injections:
- Provide only temporary benefit
- Are associated with worse long-term outcomes compared to physiotherapy or even a wait-and-see approach (Coombes et al., 2013)
- Are less effective than platelet-rich plasma (PRP) in the intermediate and longer term (Houck et al., 2019; Kemp et al., 2021)
A 2021 systematic review of systematic reviews concluded:
- Cortisone = better short-term pain relief
- PRP = better long-term pain relief and improved function (Kemp et al., 2021)
From a cost-effectiveness perspective, physiotherapy was favoured as a first-line option, while corticosteroid injections showed greater variability and lower probability of being cost-effective over 12 months (Coombes et al., 2013).
Why Might Cortisone Underperform Long Term?
Corticosteroids:
- Suppress inflammation
- Reduce pain rapidly
- Do not improve tendon structure
- May temporarily weaken tendon tissue
In degenerative tendinopathy, masking pain without improving load capacity can lead to premature return to aggravating activities, and recurrence. For this reason, corticosteroid injections are rarely our first-line strategy at Praxis.
What About PRP?
Platelet-Rich Plasma (PRP) is a biological injection derived from your own blood. It contains concentrated platelets and growth factors intended to stimulate tissue repair.
The evidence is not perfect but it is increasingly supportive in certain contexts.
A large systematic review and meta-analysis found that PRP resulted in improvements exceeding minimal clinically important difference (MCID) thresholds across commonly used outcome measures (VAS, DASH, PRTEE) from 4 weeks through to 104 weeks in many studies (Niemiec et al., 2022).
When compared directly to corticosteroid injections:
- Cortisone tends to win early
- PRP tends to win at 3–12 months (Houck et al., 2019; Kemp et al., 2021)
The 2021 review in the International Journal of Sports Physical Therapy concluded that PRP appears to be a more effective long-term treatment option for patients who have failed conservative care (Kemp et al., 2021).
Important Caveats
PRP:
- Is not a magic bullet
- Has variability in preparation methods
- Works best when combined with appropriate load rehabilitation
At Praxis, if PRP is considered, it is typically:
- For recalcitrant cases
- After structured rehab has failed
- Integrated into a progressive strengthening program
So What Actually Works Best?
High-quality evidence consistently supports physiotherapy-directed exercise programs for both short- and long-term improvement (Yelland et al., 2019; Pathan & Sharath, 2023).
Manual therapy combined with exercise has demonstrated meaningful clinical benefits compared to placebo or corticosteroid injection (Yelland et al., 2019).
There is also evidence supporting certain manipulative therapy techniques for symptom reduction (Herd & Meserve, 2008), though exercise remains the cornerstone of recovery.
Importantly, a well-designed physiotherapy program is not just:
- “Do some wrist curls”
- “Stretch your forearm”
- “Wear a brace”
Effective rehab addresses:
- Tendon load tolerance
- Grip strength deficits
- Kinetic chain contributions (shoulder and cervical loading)
- Work or sport-specific demands
- Progressive capacity building
- Assessment of cervical and local nerve contributors to pain and dysfunction
We don’t give away all the details publicly, but it’s far more nuanced than a generic exercise sheet.
Why It Takes Time
Tendons remodel slowly. Unlike muscle tissue, which may respond in weeks, tendon adaptation can take:
- 8–12 weeks for meaningful structural adaptation
- 3–6 months for substantial capacity restoration
- Longer in chronic cases
And if the condition has been present for 6–12 months already, the tissue changes are well established.
Add to that:
- Poor early management
- Repeated cortisone injections
- Ongoing load without strength progression
- High occupational demands
And recovery timelines extend further.
The Takeaway
Tennis elbow takes time because:
- It is primarily degenerative, not inflammatory (Herd & Meserve, 2008; Pathan & Sharath, 2023)
- Tendons adapt slowly
- Quick fixes often don’t address load capacity
- Short-term pain relief is not the same as long-term recovery
Cortisone may reduce pain quickly — but does not appear to be the best long-term solution (Houck et al., 2019; Coombes et al., 2013).
PRP shows more promising longer-term outcomes in persistent cases (Niemiec et al., 2022; Kemp et al., 2021) — but still works best when combined with progressive rehabilitation.
Tennis elbow rarely improves by accident — it improves with the right load, at the right time.
If you’re tired of resting, taping, or chasing temporary fixes, our team can guide you through a structured, evidence-based program designed to rebuild tendon capacity and reduce recurrence.
Book an appointment at one of our Brisbane clinics today and start moving forward with a clear plan.
Until next time, Praxis What You Preach…
📍 Clinics in Teneriffe, Buranda, and Carseldine
💪 Trusted by athletes. Backed by evidence. Here for everyone.






 A Multimodal Approach
A Multimodal Approach
