Shin Splints | Physio Guide to Medial Tibial Stress Syndrome
SUMMARY
- Shin splints are essentially an overuse injury
- Numerous factors contribute to symptoms but mainly involving the poor control of force through the lower limbs
- Important to stop symptoms to avoid developing stress fractures, which require lengthier time away from activity
- Corrective strengthening exercises, relative rest, and workload management all seem to be treatment mainstays
- Physiotherapy has a significant role to play in getting back to running and sport
SHIN SPLINTS
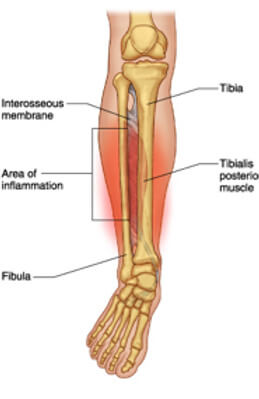
Shin splints, or as it’s referred to as in the literature, medial tibial stress syndrome (MTSS), is a common injury seen in the recreationally active and army populations. Symptoms typically consist of an aching pain to the lower medial (inside) part of the shin, that can be sharp when running or when inflamed. There can also be some pain and stiffness when you first walk around in the morning, or when you first start your activity.
Risk Factors:
Over 100 potential intrinsic risk factors of MTSS were identified in a recent systematic review [1] involving 21 different studies. Of those risk factors, nine were identified as having a moderate to strong occurrence in clinical practice. Out of these nine, the risk factors that result in the greater loads on the body (such as body mass index) or poorer acceptance of load with running were the most important.
A number of range of motion parameters were also identified. For example, larger plantar flexion range of motion (the movement of pointing your foot down) was identified. It has been hypothesized that the increased plantar flexion results in a greater likelihood of the individual landing on their forefoot rather than their rearfoot while running, possibly increasing the strain on the rear inside leg (posteromedial tibia). Forces on the inside of the shin bone explain the why pain may be present in that area.
Treatment:
Most people tend to simply rest which may decrease symptoms in the short-term, but it doesn’t address the direct cause! The condition is very commonly seen in recreational runners and not as much in your higher-level athletes. Why is this? It’s quite simple! As mentioned in our previous running blogs, the adherence to well-planned running workloads is what separates recreational runners from the competitive or non-injured. Planned training leads to adequate adaptation of the body to the demands placed upon it.
One of areas patients with shin splints focus on is poor “foot posture”. It is very common to hear the same old story, “I have shin splints because my feet are flat, I need orthotics to correct that”. The biggest problem with that approach is that not a lot of people realise that the reason that they are flat footed is not necessarily because of a defect in their feet! It may be because they have strength and control of their hips which is in turn is causing over pronation or flattening of their feet.
The diagram below demonstrates that perfectly!
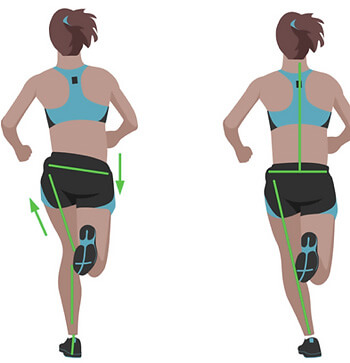

Poor hip control and strength is also a precursor for many other musculoskeletal conditions such as lower back, hip, knee and Achilles pain. So if we could reduce the risk of these outcomes occurring in the future, why wouldn’t we try!
It is possible that MTSS is a condition where the simple treatment of rest is enough to reduce symptoms. Until proven otherwise, relative rest remains the number one treatment option for reducing your symptoms. However, If addressed early, MTSS can be managed with the combination of targeted strength routines, running workloads, manual therapy and ensuring adequate recovery time between training sessions.
If you are experiencing shin splints or are looking to prevent such injuries from reoccurring, please feel free to book online or give us a call (07) 3102 3337. You’ll receive an in depth assessment and treatment plan to help you achieve your goals and run better for longer!
Till next time, Praxis what you preach.
The Praxis Team.
PREVENT | PREPARE | PERFORM
Images:
The above images are owned by the “Trainer Academy (https://traineracademy.org/) ” and used in this article with thanks.
References:
[1] Winkelmann, Z., Anderson, D., Games, K., & Eberman, L. (2016). Risk factors for medial tibial stress syndrome in active individuals: An evidence-based review. Journal of Athletic Training, 51(12), 1049-1052. 10.4085/1062-6050-51.12.13