Praxis Represents
We pride ourselves on using our skills to help athletes, weekend warriors and every day recreational exercises perform at their best. We also revel in the opportunity to tour and represent Praxis at national and international events.
In the first time in our short history, we have 3 physiotherapists out of the clinic providing their skills for Cricket Australia teams and tournaments both at home and abroad.
Stephen is looking after the Australian U19s in Colombo Sri Lanka, as recently covered in the PWYP blog: A winning Australian Cricket Side. He returns from the subcontinent on the 15th of January.
Zac, is busy down in Shepparton Victoria as a central physiotherapist for the Australia Country Cricket Championships. This competition will provide country cricketers an opportunity to play in a national carnival that will see six teams from across Australia and the East Asia Pacific (EAP) region battling across T20, OneDay and Two-Day cricket. Country cricket continues to be a tremendous nursery for talented young players including national representatives such as premier fast bowlers Andy Bichel and Shaun Tait, showing that this tournament is a viable part of the high performance pathway.
Cameron is about to embark upon two weeks in Ballarat and Bendigo as a central physiotherapist at the U18 Female National Championships. Underage National Championships are an integral part of the Australian Cricket Pathway. These Championships offer important development opportunities for our emerging stars and provide a stepping stone to further national representation. Events such as these have been the major contributor of talent to the Australian Women’s Team since its establishment helping such players as Meg Lanning and Ellyse Perry become the best in the world.
Congratulations to our three physiotherapists and we look forward to seeing them back in clinic soon!
Till next time,
Prevent. Prepare. Perform
Team Praxis

Causes and Risks
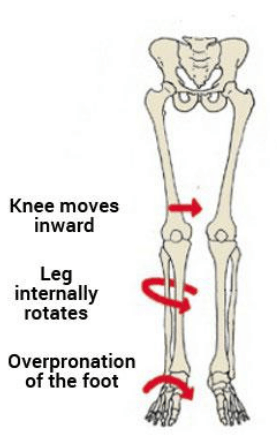
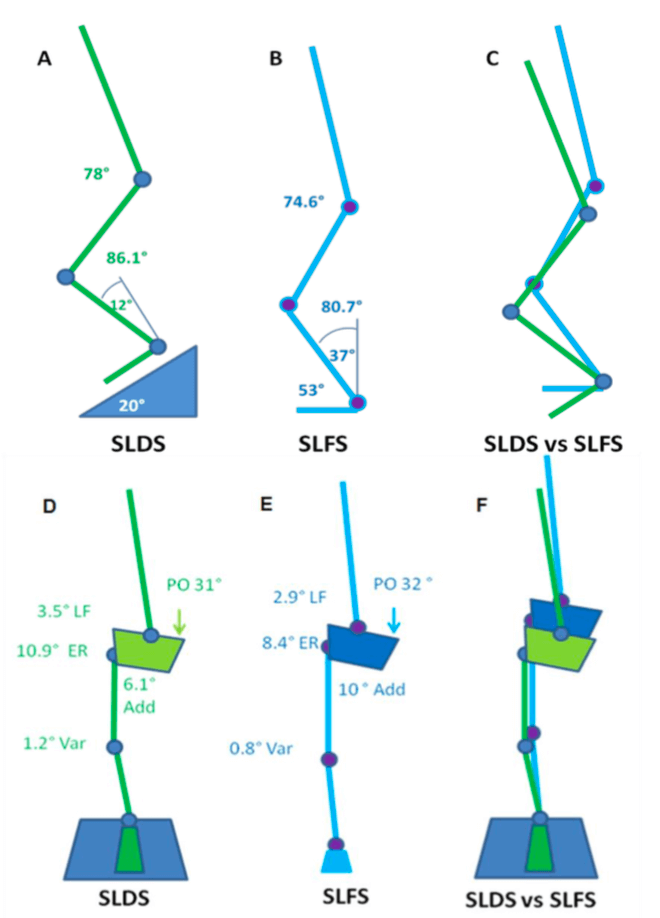
Achilles tendinopathy typically results from a combination of intrinsic and extrinsic factors. Intrinsic factors include age, reduced flexibility, reduced calf strength / endurance and poor lower limb biomechanics. Extrinsic factors encompass inappropriate footwear, training errors (such as a spike or change in workload), and inadequate warm-up or cool-down routines. Additionally, individuals with systemic conditions like diabetes or rheumatoid arthritis may be more prone to developing Achilles tendinopathy. Understanding these factors is crucial for tailoring treatment plans to address the root causes and minimize the risk of recurrence. But in the most reductionist of terms, Achilles tendinopathy develops due in large part due to a mismatch between loading and the capacity of the tissue.
Diagnosis and Assessment
Accurate diagnosis of Achilles tendinopathy relies on a thorough clinical examination and patient history. Physiotherapists employ various assessment techniques, such as palpation, functional tests, and imaging modalities like ultrasound or MRI, to evaluate the severity and extent of the condition. A self administered questionnaire (VISA-A) can help evaluate symptoms and their effect on physical activity and in turn, the clinical severity. This comprehensive assessment helps determine the appropriate treatment approach, including targeted exercise programs, manual therapy, and other interventions.
Treatment Strategies
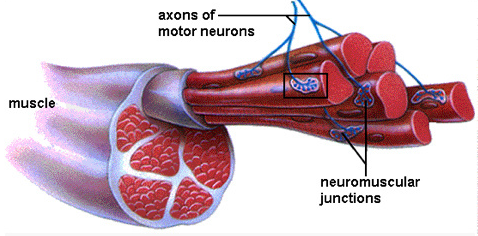
Physiotherapy plays a pivotal role in the management of Achilles tendinopathy. Treatment strategies focus on reducing pain, promoting healing, and improving function. These will include calf strengthening exercises, stretching routines and activity modification as frontline options. Moreover, physiotherapists can guide patients in proper footwear selection, gait retraining, and implementing preventive measures to minimize the risk of reinjury.
Rehabilitation and Prevention
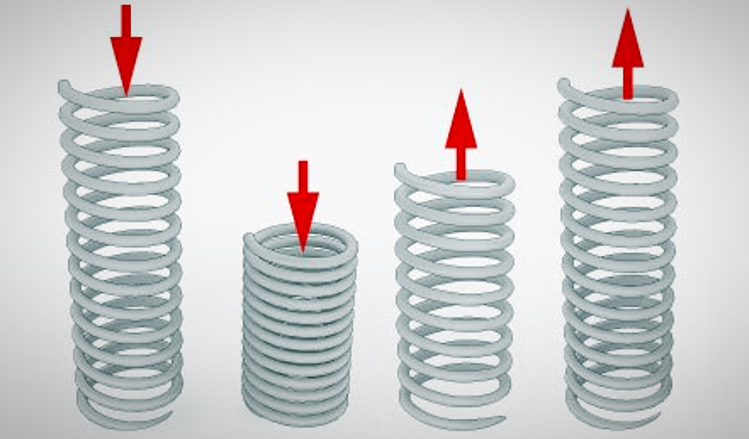
Rehabilitation programs are essential for individuals recovering from Achilles tendinopathy. Gradual progression of exercise intensity, functional training, and sport-specific drills enable patients to regain strength, flexibility, and proprioception while minimizing the risk of relapse. Educating patients on proper warm-up and cool-down routines, appropriate footwear selection, and regular monitoring of training loads can significantly contribute to preventing Achilles tendinopathy in the future. One of the common errors patients make is making rehabilitation too easy, or returning to sport too quickly. Again, physiotherapy play a pivotal role in ensuring you undertake a graduated return to loading as the application of mechanical stress to the Achilles tendon promotes tendon healing and remodeling.
Conclusion
Achilles tendinopathy requires a comprehensive approach for effective management. As physiotherapists, our knowledge and expertise are invaluable in helping you overcome this condition and return to their active lifestyles. To discuss your Achilles issues with us to get you back to what you love doing, book online with Praxis today.
Until next time, Praxis What Your Preach.
Team Praxis