JOINT ANGLES (KINETMATICS:)
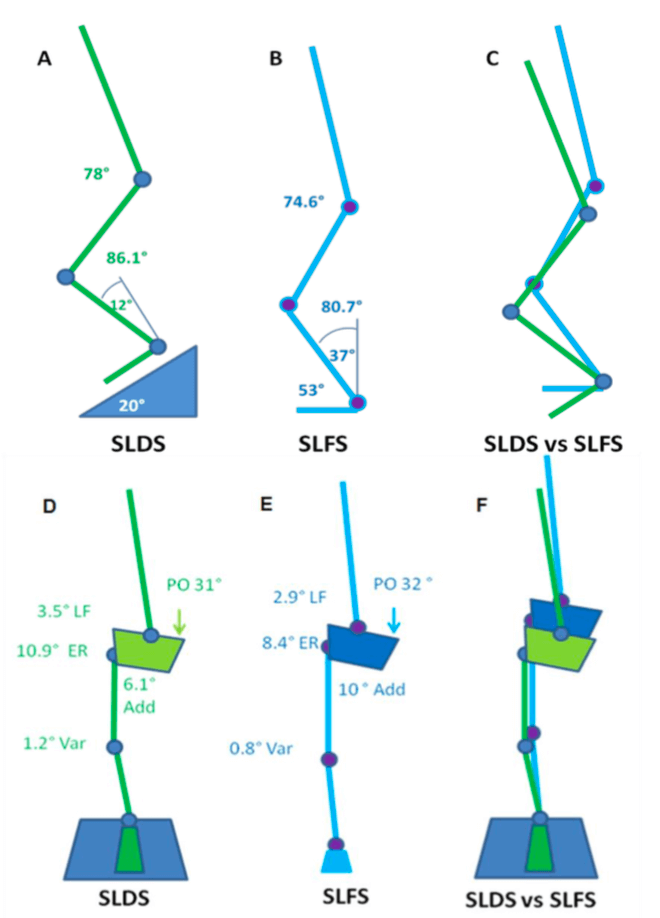
A picture tells a thousand words so in the interests of brevity, the stick squat figure is essentially a summary of two years of work.
So what this means, when someone performs a SLS on a flat surface, relative to a decline surface they tend to have:
- A more upright torso
- More rotation of the pelvis toward the weigh bearing (WB) limb
- Reduced flexion but more adduction and internal rotation of the thigh on the WB hip (pelvic close to femur)
- Less flexion of the knee but the same position relative to the foot as you look from the front (known as frontal plane knee excursion) at the bottom of range
- Reduced internal rotation of the shin
- Reduced ankle flexion
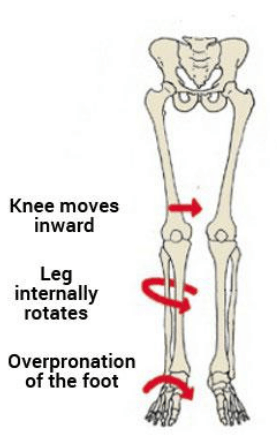
Essentially, in a flat squat you tend to ‘corkscrew’ your pelvis and adopt the medial collapse position much more easily than in the decline squat position. This may because of ankle range of motion issues as well as the ability to adequately recruit pelvic musculature. Yep – two years to get that!
STRENGTH AND MOVEMENT:
My results demonstrated a tendency for the pelvis to remain increasingly level with greater hip abduction strength. However, the relationship between strength and the pelvis was observed in the decline condition but not the flat condition. This may be due to hip abduction was shown to be significantly less (more neutral) in the SLDS which seemingly promoted greater muscle activation and subsequent control of pelvis. The self selection of squat depth may have also been a critical factor in finding as those with weak hips may have squatted deep to adopt maladaptive positions. Previous research has indicated that the hip abductors and external rotators play an important role in lower extremity alignment as they assist in the maintenance of a level pelvis [9] and are capable in balancing a number of biomechanical forces in the body [10].
Interestingly, there were no significant relationships observed between hip abduction strength and knee valgus (knee falling in) for both squatting conditions. There was however a trend between hip abduction strength and knee valgus which supported previous research. It is keeping with the assumption that increased knee valgus might also be associated with reduced hip abduction and external rotation strength [11].
SUMMARY:
- To maximise athletic function, particularly in sports such as soccer, netball and AFL, stability through the pelvis and hips, proximal lower limb, spine and abdominal structures is required [12].
- The importance of pelvis stabilisation for lower extremity injury prevention [13] particularly the knee [14-17] has been well documented in the literature.
- Adequate lumbopelvic-femur strength and muscle function may conceivably reduce exposure to other intrinsic risk factors such as inefficient force attenuation, unstable movement patterns and lower limb malalignments during activity [18, 19].
- Ankle flexibility may also be a factor in lower limb physical resilience and injury prevention.
- Support for the previous statements has been demonstrated in the relationships between hip strength measures and kinematics within selected results of my study.
There you have it. Two years of my life summarised to a few paragraphs. From a personal perspective, I took away from my research experience to be always questioning why we do things and see if there is someone out there who has answered the questions we seek. Finally, don’t overcook chicken – Ramsay doesn’t like it.