Shoulder Stabilisation and Bankart Repair: Your Path Back to Sport
Recovering from a shoulder stabilisation surgery, particularly a Bankart repair, can feel like navigating a winding trail. At Praxis Physiotherapy, we understand that athletes don’t just want to heal – they want to return stronger, more confident, and ready for action. This blog explores the key milestones in overhead and contact sport rehabilitation and the compelling evidence that supports structured physiotherapy.
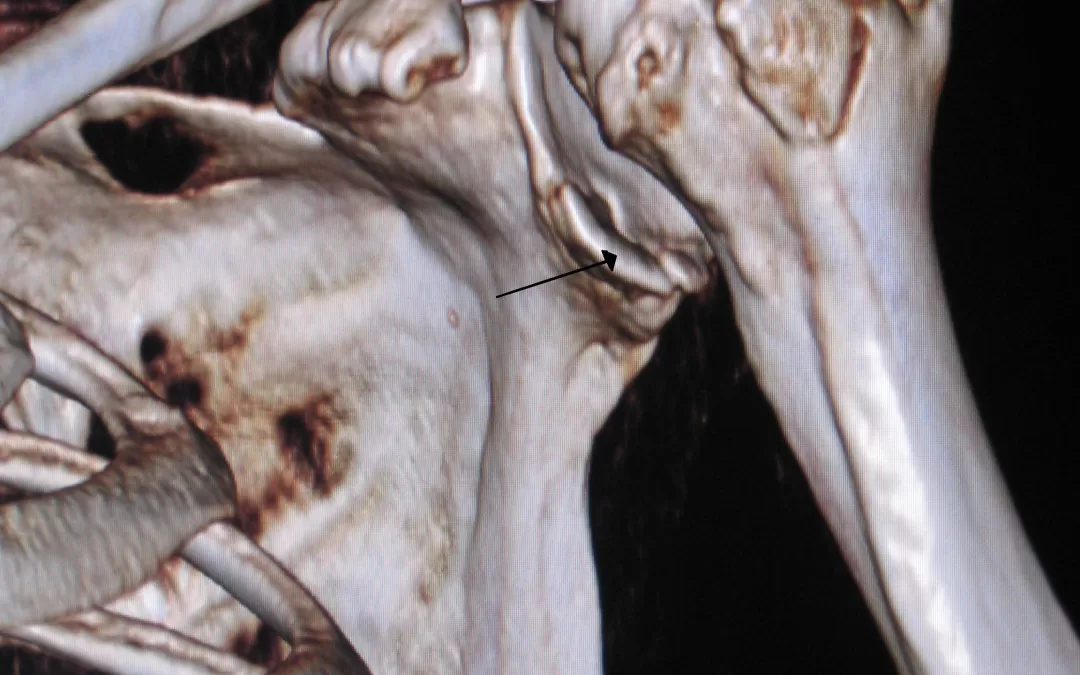
Understanding Shoulder Stabilisation and Bankart Repair
The Bankart repair is a surgical intervention for traumatic anterior shoulder dislocations, which are most common in young, active populations – particularly those involved in contact or overhead sports. This procedure reattaches the torn labrum to the glenoid, restoring joint stability. While the surgery addresses structural instability, it is only the first step. Rehabilitating the shoulder to perform under high-stress, dynamic sporting conditions is where physiotherapy becomes crucial (Coyle et al., 2022).
Rehabilitation Phases: Beyond the Basics
Rehabilitation after Bankart repair generally progresses through four overlapping phases:
1. Protection & Early Mobility (0–6 weeks)
Initial goals include reducing pain and inflammation while protecting the repair. Gentle passive and assisted range-of-motion exercises begin, with sling use gradually tapered.
2. Strength Building (6–12 weeks)
Isometric and light resistance training begins. Scapular control and rotator cuff strengthening are vital. Coyle et al. (2022) found wide variability in when strengthening begins, from 1 to 12 weeks, underscoring the importance of tailored plans.
3. Advanced Control & Load Tolerance (12–20 weeks)
This phase introduces overhead activity simulation, plyometrics, and proprioceptive drills. Neuromuscular training improves shoulder resilience, especially under rapid direction changes and contact stress (Ialenti et al., 2017).
4. Return to Sport (20+ weeks)
Athletes progressively re-engage in sport-specific drills, initially non-contact, then full-contact scenarios. Full return to competitive play often occurs around 5–6 months, but timelines vary based on sport demands (Kasik et al., 2019).
The Evidence: Why Physiotherapy Matters
- A systematic review by Rossi et al. (2021) revealed that 27% of athletes failed to return to sport post-surgery. Most cited fear of reinjury, not physical limitation, as the main barrier. Targeted rehab can address both physical readiness and confidence.
- Kim et al. (2023) showed that factors such as shoulder strength, proprioception, and psychological readiness were predictive of successful return. Structured physiotherapy addresses all three.
- The American Journal of Sports Medicine confirms that progressive loading, especially for overhead and contact tasks, enhances long-term outcomes and reduces recurrence rates (Kim et al., 2023).
- Alsomali et al. (2021) and Stone & Pearsall (2014) agree that sport-specific milestones are crucial, with a general return-to-contact timeline of 16–24 weeks depending on the sport.
Back in the Game: What Sets Our Approach Apart
At Praxis Physiotherapy, our shoulder rehabilitation programs don’t just follow protocols – they evolve with the athlete. We incorporate evidence-based practices and tailor each phase to your sport, position, and performance goals. Whether you’re a rugby forward or a volleyball setter, our rehab plan adapts to your demands.
We emphasise:
- Early and progressive exposure to overhead mechanics
- Integrated neuromuscular training for dynamic stability
- Gradual and safe return-to-contact drills
- Psychological readiness assessments to overcome fear of reinjury
Summary Timeline for Return to Sport
| Phase | Timeframe | Focus |
|---|---|---|
| Protection & Early Mobility | 0–6 weeks | Pain control, protected motion |
| Strength & Motor Control | 6–12 weeks | Rotator cuff & scapular strengthening |
| Overhead & Contact Prep | 12–20 weeks | Plyometrics, proprioception, advanced drills |
| Return to Sport | 20–26+ weeks | Gradual return to contact and full intensity |
Final Thoughts: Your Comeback Starts with the Right Team
Recovering from shoulder stabilisation surgery is not just about healing – it’s about coming back better. Evidence clearly shows that structured, progressive physiotherapy is essential for returning to sport safely and confidently.
At Praxis Physiotherapy, we’re here to guide that journey every step of the way. If you are ready to get started, book online today.
Until next time, Praxis What You Preach…
📍 Clinics in Teneriffe, Buranda, and Carseldine
💪 Trusted by athletes. Backed by evidence. Here for everyone.
References
- Coyle, M., Jaggi, A., Weatherburn, L., Daniell, H., & Chester, R. (2022). Post-operative rehabilitation following traumatic anterior shoulder dislocation: A systematic scoping review. Shoulder & Elbow, 15(5), 554–565.
- Ialenti, M. N., Mulvihill, J. D., Feinstein, M., Zhang, A. L., & Feeley, B. T. (2017). Return to play following shoulder stabilization: A systematic review and meta-analysis. Orthopaedic Journal of Sports Medicine, 5(9)
- Kasik, C. S., Rosen, M. R., Saper, M. G., & Zondervan, R. L. (2019). High rate of return to sport in adolescent athletes following anterior shoulder stabilisation: A systematic review. Journal of ISAKOS, 4(1), 43–50.
- Kim, M., Haratian, A., Fathi, A., Kim, D. R., Patel, N., Bolia, I. K., … & Weber, A. E. (2023). Can we identify why athletes fail to return to sports after arthroscopic Bankart repair? A systematic review and meta-analysis. The American Journal of Sports Medicine, 51(9), 2480–2486.
- Rossi, L. A., Tanoira, I., Brandariz, R., Pasqualini, I., & Ranalletta, M. (2021). Reasons why athletes do not return to sports after arthroscopic Bankart repair: A comparative study of 208 athletes with minimum 2-year follow-up. Orthopaedic Journal of Sports Medicine, 9(7)
- Alsomali, K., Kholinne, E., Nguyen, T. V., Cho, C.-H., Kwak, J.-M., Koh, K.-H., & Jeon, I.-H. (2021). Outcomes and return to sport and work after open Bankart repair for recurrent shoulder instability: A systematic review. Orthopaedic Journal of Sports Medicine, 9(10)
- Stone, G. P., & Pearsall, A. W. (2014). Return to play after open Bankart repair: A systematic review. Orthopaedic Journal of Sports Medicine, 2(2),




 A Multimodal Approach
A Multimodal Approach





